“Why does everything I love hurt me?”
~Homer Simpson, The Simpsons
Sometimes, you get a sunburn because you stayed out too long. Other times, you get a sunburn because your skin has decided to violently overreact to a mild sunny Tuesday afternoon.
This is sun sensitivity (photosensitivity / photosensitization). It’s not a standard burn; it’s a chemical conspiracy.
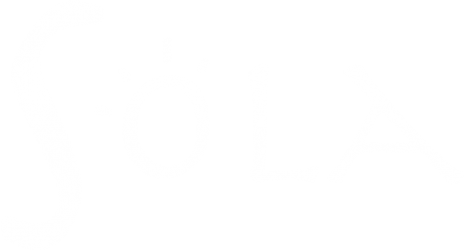
How It Works: The “Magnifying Glass” Effect
Photosensitization happens when certain chemicals (let’s call them “Skin Traitors”) absorb UV rays and amplify them. It turns your skin into a solar panel that is a little too enthusiastic.
- Endogenous Traitors: Chemicals produced inside your body (because sometimes your own metabolism hates you).
- Exogenous Traitors: Chemicals introduced from the outside (medications, perfumes, or that lime you squeezed into your drink).
Photosensitization is not genetic the way skin type is. Anyone can get hit with it – any age, any gender, any skin tone – even if you’ve handled sunshine like a champ your whole life.
The Two Flavors: Toxic vs. Allergic
Sun sensitivity reactions mostly fall into two buckets:
Phototoxic Reactions (The “Instant Sizzle”)
- Vibe: This is the most common type. Think Super-Sunburn.
- Timing: Happens fast (minutes to hours after sun exposure).
- Look: Exaggerated sunburn: redness, burning/stinging, sometimes peeling, swelling and blisters. Confined strictly to the areas the sun hit.
- Cause: Usually oral or systemic drugs. The drug literally interacts with light to damage cells. Dose-dependent: more drug + more UV = more damage.
- Caution: Can leave behind long-lasting dark patches once they heal.
Photoallergic Reactions (The “Delayed Grudge”)
- Vibe: “Slow burn” immune reaction.
- Timing: Slow (24–72 hours). This is your immune system filing a formal complaint three days after the crime.
- Look: Itchy, scaly, eczema-like rash. Unlike the toxic version, this rash has no respect for boundaries and can spread to areas that were covered by clothes.
- Cause: Usually topical stuff (certain sunscreens, fragrances, antiseptics, some topical NSAIDs). UV light changes the chemical structure of the product, and your immune system decides this new molecule is an enemy combatant.
- Caution: Can become chronic, with flares long after you stop using the original trigger.
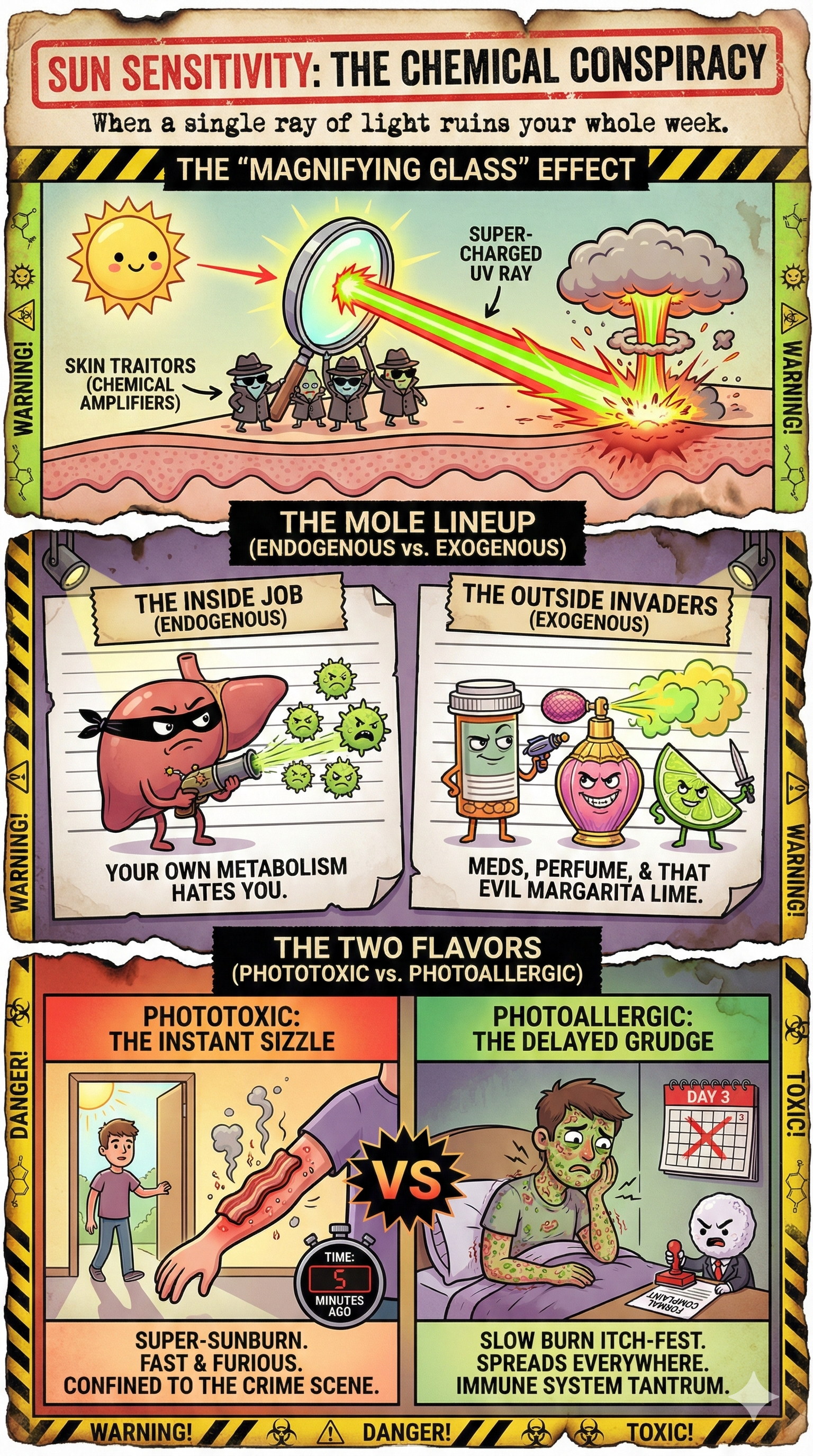
The Usual Suspects (Common Culprits)
Everyday items can turn on you. Here is the lineup of potential betrayers:
The Medicine Cabinet
- Antibiotics/antifungals: Tetracyclines, doxycycline, sulfonamides, voriconazole, ketoconazole, itraconazole, etc.
- Anti-inflammatories (NSAIDs): Ibuprofen, naproxen, piroxicam. People often miss the connection because they don’t take them daily.
- Diuretics & heart meds: Keeping your blood pressure down, but your burn risk up.
- Antidepressants/antipsychotics: tricyclics, some SSRIs, herbal St. John’s Wort, and especially phenothiazines like chlorpromazin.
- Oral retinoids: Isotretinoin, acitretin; they create brand-new baby skin with zero defense stats. Great for acne, terrible for beach days.
Moral of the story: that tiny pill can dramatically lower your “time to burn” without telling you.
The Vanity Trap (Topicals)
- Retinols & acids: We use them to look younger, but they thin or irritate the skin; basically removing the roof before a storm.
- Old-school sunscreens: Those with PABA or certain benzophenones. Modern formulations are better, but sensitivity can still happen.
- Skin-care treatments, perfumes, and oils: Berloque dermatitis is a classic example; some perfumey things (especially with bergamot or musk ambrette) react with the sun and leave brown streaks on your neck or chest. You smell expensive, but you look streaky.
The Salad of Doom (Plants & Foods)
- Psoralens: Found in celery, parsley, parsnip, figs, “wild parsnip,” giant hogweed, citrus (especially lime, bergamot, grapefruit, and bitter orange).
- When eaten: Normal amounts are usually fine. Huge amounts + strong sun can slightly increase burn risk, but usually less dramatically than meds.
- When sap or juice hits your skin: UV activates the psoralens in the sap.
- Celery is an occupational hazard for agricultural workers; hands and forearms often pay the price.
- Lime juice + sun: can cause “margarita dermatitis” on the hands and arms of bartenders, beach-party people, and anyone squeezing limes outdoors.
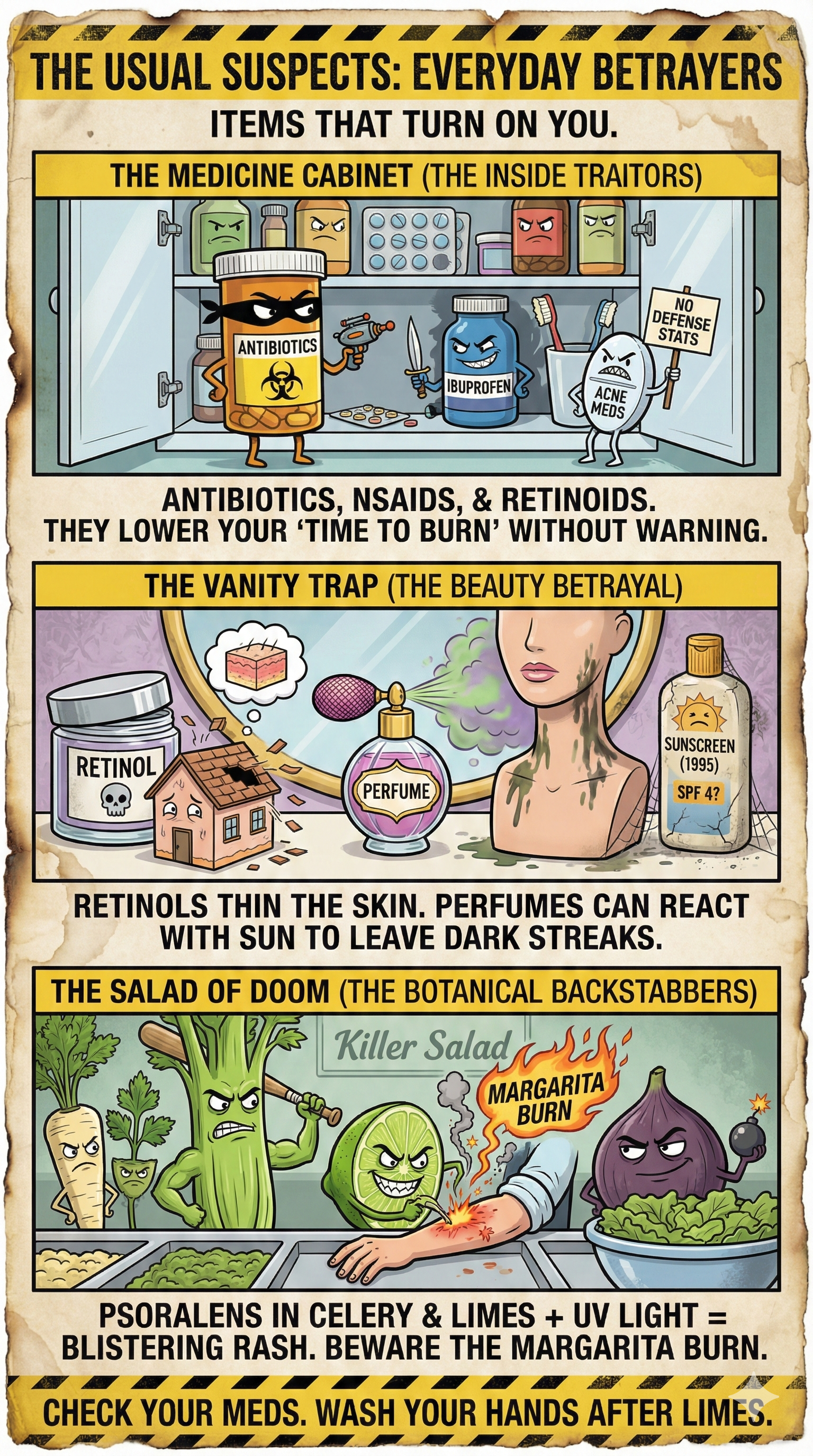
Medical Conditions: When Biology is Unfair
Some diseases come with pre-installed sun sensitivity:
- Lupus (SLE): The “Vampire Rule” applies. Even UVA through a window can trigger a flare with rashes and systemic symptoms.
- Porphyria: Metabolic disorders where sunlight equals blistering and pain after very little exposure.
- Albinism & XP (xeroderma pigmentosum): Genetic conditions where the body either forgot to make melanin or forgot how to repair UV damage. Both equal extreme UV sensitivity.
- Rosacea: Chronic facial redness that loves to flare in the sun.
- Melasma: Stubborn dark patches on the face and other exposed areas that get worse with every sunny day.
Survival Guide: How Not to Sizzle
Prevention (The “Don’t Be Stupid” Phase)
- Check your meds: Ask your pharmacist, “Will this pill turn me into a vampire?”
- Wash your hands: After making guacamole or cocktails outdoors, wash your hands. Lime juice + sun = designer blisters.
- The window trap: If you have lupus or known photosensitivity, remember: UVA penetrates glass. You are not automatically safe just because you’re indoors.
- Use physical protection: On photosensitizing meds? Use broad-spectrum sunscreen, UPF-rated clothing, wide-brimmed hats, sunglasses, shade (umbrellas, trees, literally anything).
Treatment (The “I Messed Up” Phase)
- Treat it like a sunburn: But with extra suspicion.
- Cool down: Cold showers, damp towels. No ice. Frostbite on a burn is a humiliating combo injury.
- Hydrate: Drink water (and maybe electrolytes). Your skin and body are thirsty.
- The forbidden bubble wrap: If you get blisters, DO NOT POP THEM. They are nature’s sterile bandage.
- The “Hell Phase” (itching): Do not scratch. Use a thin layer of hydrocortisone (unless your doctor says otherwise). Scratching leads to infection, and nobody wants a festering arm.
- Watch for red flags: Large blistered areas, rapidly spreading rash, fever, chills, nausea, weakness = time to see a doctor, not Google.
- Avoid further sun until it settles: Going back into bright sun mid-reaction is like pouring gasoline on a campfire and calling it “optimistic.”
Severe photosensitive reactions can leave behind dark spots (hyperpigmentation) that last for months. And repeatedly frying your DNA with phototoxic drugs + UV does your long-term skin cancer risk zero favors.
TL;DR: If you’re on antibiotics, retinoids, mystery meds, or squeezing limes outdoors, maybe befriend the umbrella.

END OF CHAPTER